The Fascinating Science Behind How Medicines Actually Work
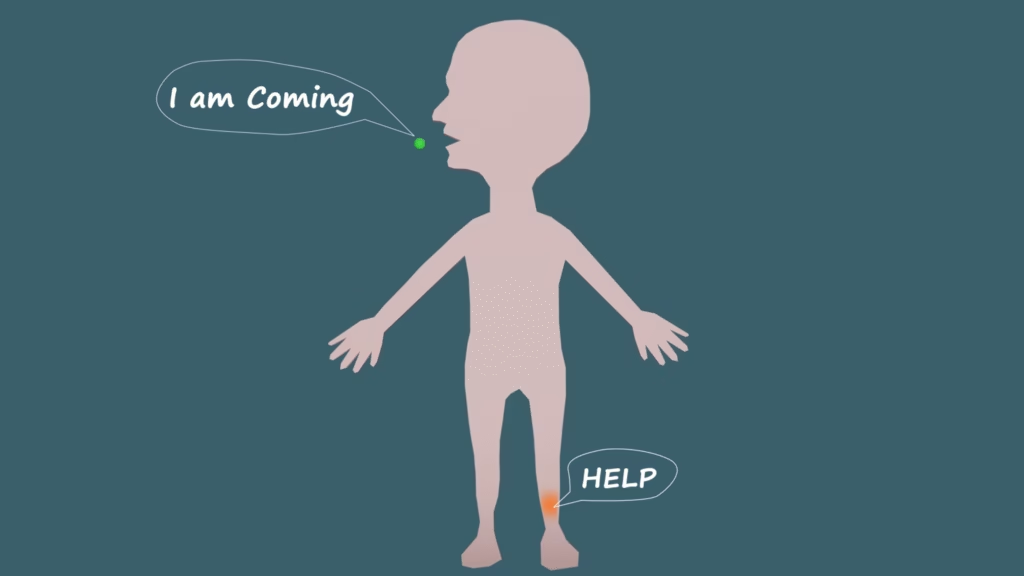
How Do Medicines Know Where to Heal?
When you swallow a pill, have you ever thought about what really happens next?
How does that tiny tablet you take for a headache, fever, or infection travel inside your body, find the right spot, and actually fix the problem?
Does a medicine somehow know where the pain is?
Does it have a brain or memory that tells it where to go?
The real answer is both fascinating and surprisingly simple.
Medicines don’t have intelligence — they rely on biology, chemistry, and a bit of clever human design.
Let’s take a slow, detailed journey inside the body to understand how medicines work — from the moment you take them until they leave your system.
Step 1: The Medicine Enters Your Body
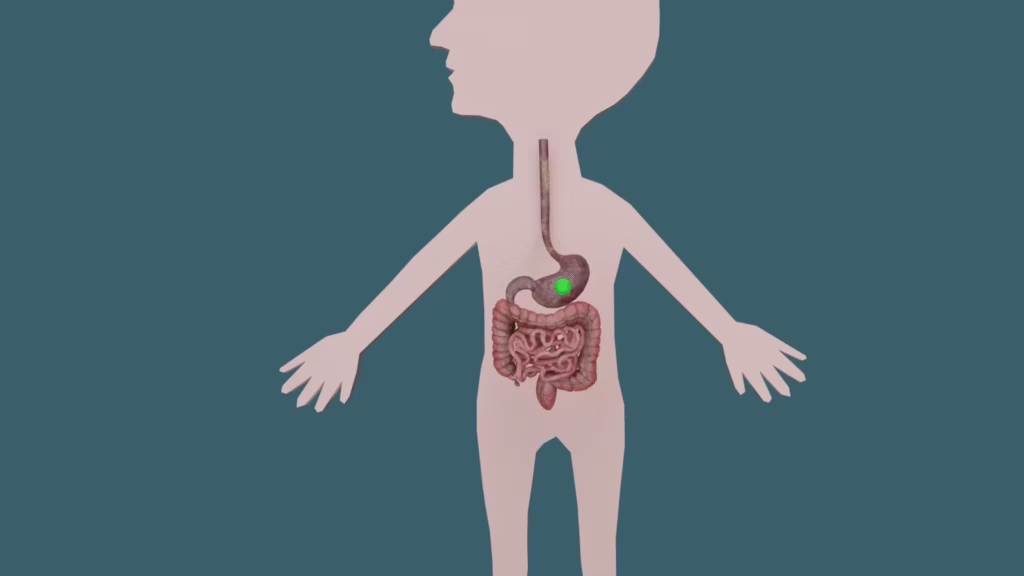
Most medicines begin their journey the same way — through your mouth.
They can come in many forms: tablets, capsules, or liquid syrups.
When you swallow a tablet, it travels down your throat, through the esophagus (also called the food pipe), and reaches your stomach.
Inside your stomach, powerful gastric juices start to break down the outer coating of the tablet.
However, not all medicines are designed to dissolve here.
Some have special coatings (called enteric coatings) that resist stomach acid so the drug can safely reach the small intestine, where it can be absorbed.
But oral medicines are not the only way drugs enter your body:
Injections deliver medicine directly into the bloodstream or muscle.
Inhalers send medicine straight to your lungs (common for asthma).
Eye or ear drops target specific organs.
Creams and gels are absorbed through the skin for local action.
No matter how a medicine enters your system, its ultimate goal is always the same:
to reach its target, do its job, and help your body heal.
Step 2: Absorption — Entering the Bloodstream
After the medicine breaks down in the stomach, the smaller molecules move into the small intestine.
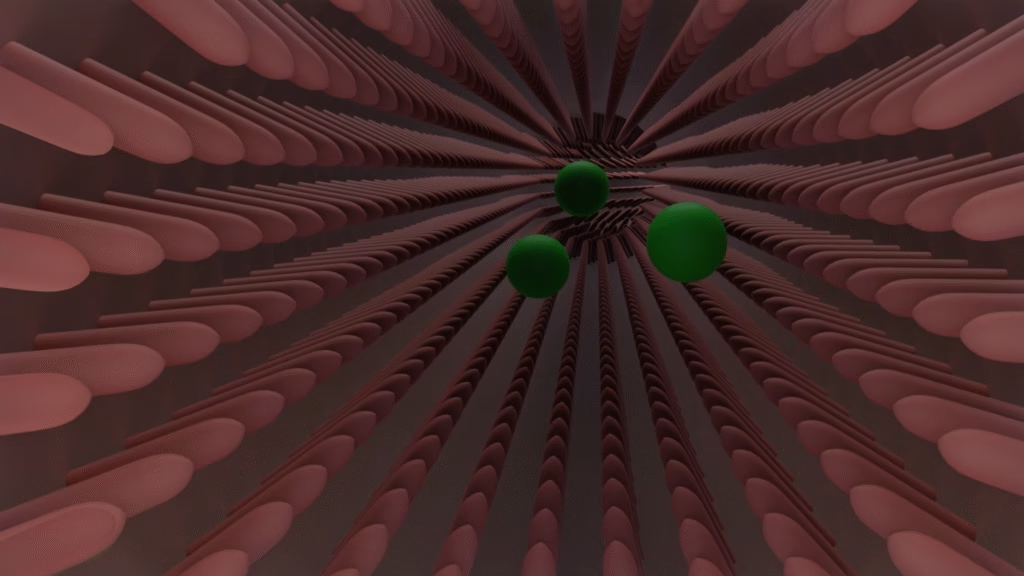
This part of your digestive system has an inner lining full of tiny folds and finger-like projections called villi, making it look and act like a sponge.
The villi increase the surface area dramatically, allowing nutrients — and medicines — to be absorbed efficiently.
The drug molecules then cross the intestinal wall and enter the bloodstream.
This crucial process is called absorption, and it marks the point where the medicine officially becomes available to your whole body.
However, not all drugs are absorbed equally well.
Some drugs are fat-soluble, meaning they dissolve better in fat, while others are water-soluble.
The drug’s chemical properties — its size, charge, and solubility — determine how quickly and effectively it enters the blood.
Once absorbed, the medicine now begins to circulate throughout your body, carried by your blood — just like cars traveling on a massive network of highways.
Step 3: Distribution — Traveling Through the Body
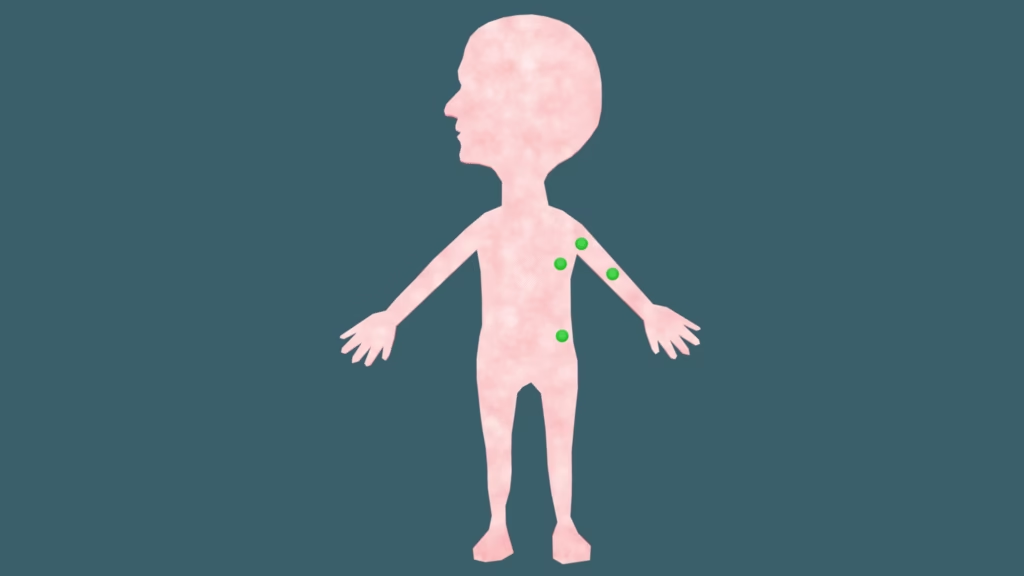
Your bloodstream acts as a transport network, carrying the medicine to different organs and tissues.
But here’s an interesting detail: not all of the medicine floating in your blood is free to act.
Some of it binds to plasma proteins like albumin — these proteins act a bit like “taxis” that hold onto the drug molecules.
This bound portion acts as a storage form, while the unbound (free) portion is the one that actually performs the therapeutic work.
The body constantly maintains a balance between the bound and unbound drug — this ensures that the medicine’s effect lasts for a predictable amount of time.
Certain organs, such as the liver, kidneys, brain, and fat tissue, receive more blood than others, so the drug reaches these places faster.
Other tissues get less, so the medicine takes longer to arrive there.
This distribution process depends on many factors:
The drug’s solubility (fat vs water)
Blood flow to different tissues
Protein binding
Barriers like the blood-brain barrier, which protects your brain from harmful chemicals
Step 4: Metabolism — The Liver Gets to Work

As the medicine circulates, your body begins to process it.
This step is known as metabolism, and it mostly happens in the liver — your body’s chemical factory.
The liver contains special enzymes (especially a group called cytochrome P450) that break down medicines into metabolites.
Sometimes these metabolites are active (they still have an effect), and sometimes they are inactive waste products ready to be removed.
This process is important for two reasons:
It helps make the medicine more water-soluble, so it can be excreted easily by the kidneys.
It prevents medicines from building up to dangerous levels in your body.
For drugs taken orally, there’s a special challenge called first-pass metabolism — meaning that before the drug reaches the bloodstream, it passes through the liver where a portion of it is broken down.
That’s why the effective dose in your body may be smaller than the amount you originally swallowed.
Step 5: Excretion — Leaving the Body
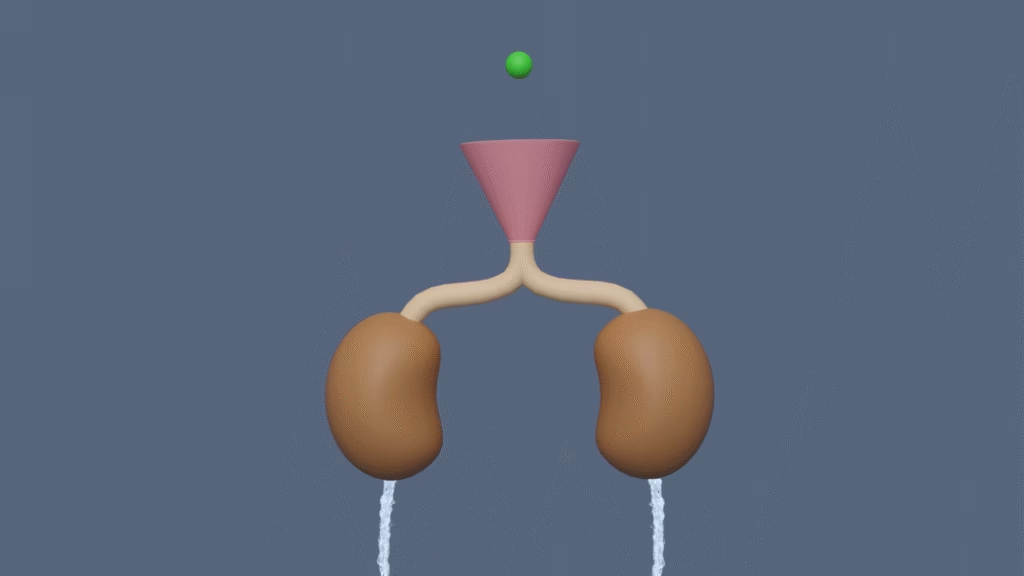
After the medicine has done its job, your body needs to remove it.
This is called excretion, and it mainly happens through your kidneys.
The kidneys act like natural filters, cleaning your blood by removing waste, excess water, and drug metabolites.
These waste products are then eliminated in urine.
Some drugs or their byproducts are excreted through other routes too:
Bile and feces
Sweat
Breath (for some gases and alcohol)
Breast milk (important in drug safety for nursing mothers)
The entire journey — absorption, distribution, metabolism, and excretion — is summarized by scientists as ADME, which defines how a medicine behaves in the body.
How Does the Medicine “Know” Where to Work?
Now comes the most fascinating question.
If you take a painkiller for your hand, how does it know that the pain is in your hand and not in your foot or back?
The simple answer:
It doesn’t know at all.
Medicines don’t think, sense, or choose.
Once they enter your bloodstream, they spread throughout your entire body.
They only work where their chemical structure fits — and that’s where biology does the magic.
The Lock-and-Key Mechanism
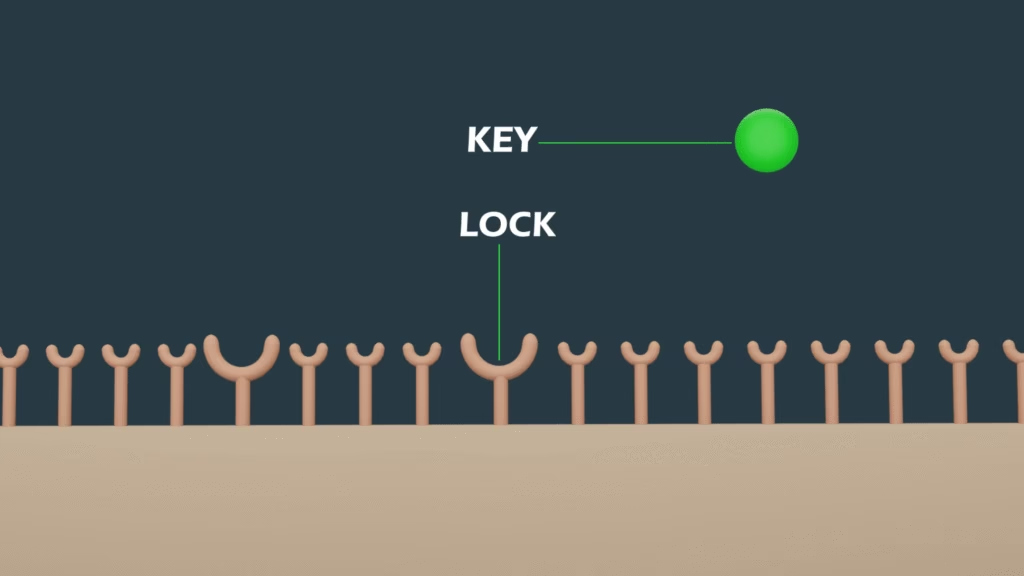
Every cell in your body has special structures on its surface called receptors.
Think of these receptors as tiny locks.
Each medicine molecule has a specific shape, like a key.
When the right key fits into the right lock, it triggers a specific action — this could be:
Starting a reaction (activating a receptor)
Blocking a reaction (inhibiting an enzyme)
Modifying a signal (modulating a process)
If the medicine doesn’t find any matching locks, it simply keeps circulating until it’s metabolized and excreted.
This lock-and-key model is one of the most powerful concepts in pharmacology.
It explains how drugs can be so specific — and why they sometimes cause side effects if they fit other, unintended “locks” in the body.
Example: How Painkillers Like Ibuprofen Work
Let’s revisit our example of Ibuprofen, one of the most common non-steroidal anti-inflammatory drugs (NSAIDs).
Your body naturally produces chemicals called prostaglandins, which are responsible for pain, inflammation, and fever.
These prostaglandins are made by enzymes called cyclooxygenase (COX-1 and COX-2).
Ibuprofen works by inhibiting these enzymes.
In simpler words, it blocks the “factory” that produces pain and inflammation signals.
Once prostaglandin production drops, you feel less pain and swelling — whether that’s in your hand, your back, or anywhere else those chemicals were active.
Because Ibuprofen affects both COX-1 and COX-2 enzymes, it can also cause side effects such as stomach irritation — since COX-1 helps protect the stomach lining.
That’s why doctors often recommend taking it with food or using safer alternatives for long-term use.
Example: How Antibiotics Find Bacteria
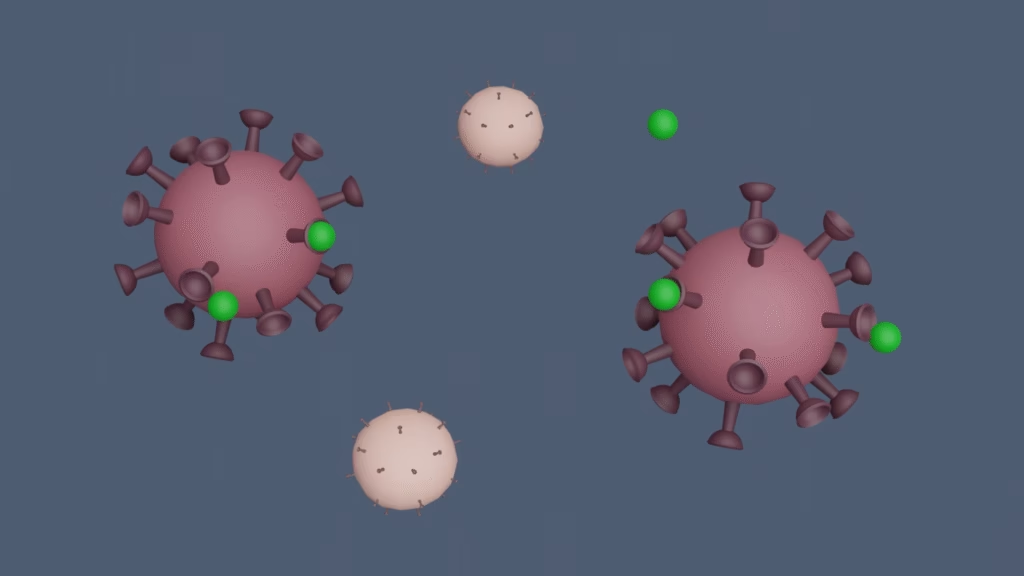
Now imagine you’re taking an antibiotic for an infection.
Antibiotics are clever chemical weapons — but they still don’t “think.”
They target specific structures or processes that exist in bacteria but not in human cells.
For example:
Penicillin stops bacteria from building cell walls.
Tetracyclines block bacterial protein production.
Ciprofloxacin interferes with bacterial DNA replication.
Because human cells don’t have these same structures, antibiotics can kill bacteria without harming your own cells — at least when used properly.
Other Ways Medicines Work

Not all medicines target enzymes or receptors. Some work through different mechanisms:
Pain-relievers (like paracetamol) may act directly on the brain’s pain-control centers.
Antihistamines block histamine receptors to reduce allergies.
Antidepressants alter neurotransmitter levels in the brain.
Vaccines train your immune system to recognize and destroy future infections.
Hormones (like insulin) replace or balance substances your body lacks.
Every medicine has a unique pathway, but they all rely on the same basic biological principles — traveling through the blood, finding the right “lock,” triggering a response, and eventually being cleared.
Why Medicines Need Regular Doses
Medicines don’t stay in your body forever.
After you take a dose, its concentration in your blood slowly decreases as your liver and kidneys do their job.
The rate of this decrease is measured as the half-life — the time it takes for the concentration of the drug in your body to reduce by half.
Some drugs have a short half-life (just a few hours), while others last for days.
That’s why you often see instructions like:
“Take every 6 hours”
“Take twice a day”
“Take once daily”
These schedules make sure the drug level in your body stays high enough to be effective but not high enough to cause toxicity.
What Happens If You Take Too Much?
If you take a higher dose than prescribed, your liver and kidneys can become overloaded.
This can lead to toxicity or drug overdose.
For example:
Too much paracetamol (acetaminophen) can cause liver damage.
Overuse of NSAIDs like Ibuprofen can harm the stomach or kidneys.
Excess antibiotics can disrupt gut bacteria and lead to resistance.
That’s why proper dosage, timing, and doctor guidance are so important — even though over-the-counter medicines look harmless.
The Science Behind It All — ADME in Summary
Pharmacologists describe the journey of any drug through four key stages, often abbreviated as ADME:
| Stage | Process | Key Organ / Function |
|---|---|---|
| A | Absorption | Drug enters the bloodstream (intestine, lungs, skin, etc.) |
| D | Distribution | Drug travels throughout the body via blood |
| M | Metabolism | Liver breaks down the drug into metabolites |
| E | Excretion | Kidneys and other organs remove waste |
Each stage affects how well a medicine works, how long it lasts, and how often you need to take it.
Conclusion: It’s Not Magic — It’s Science!

It’s not a tiny robot searching for the problem, and it’s not a machine that can think.
It’s pure chemistry and biology — working together in perfect harmony.
Your body’s amazing systems — from the digestive tract to the bloodstream, from the liver to the kidneys — handle every step with incredible precision.
Medicines don’t know where to go.
They simply move with your blood, and the natural laws of biology decide where they fit and how they act.
It’s not magic.
It’s science — quietly, beautifully, and brilliantly at work inside you.
About the Author
This article was prepared by the IRA Studios editorial team, creators of high-quality 3D educational visualizations designed to simplify complex ideas through clear and engaging visuals.
Watch the Full 3D Animation
To explore all of these processes in 3D, check out our detailed 3D Animation video.
Want to learn more through visual storytelling? Check out our detailed 3D explanation blog on Understanding Heart Attacks: A 3D Explanation of Causes, Symptoms, and Prevention
Useful Links