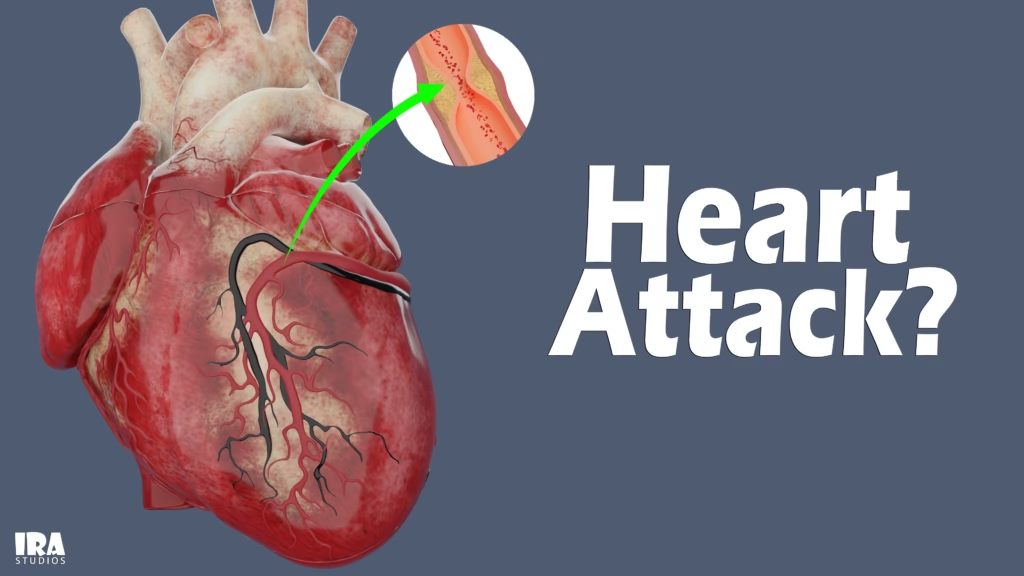
Heart Attack explained with 3D Visuals
According to WHO every year, cardiovascular diseases kill an estimated 19.8 million people worldwide, accounting for roughly 32% of all deaths. Of those cardiovascular deaths, about 85% are due to heart attacks (also called myocardial infarctions) and strokes.
Given those staggering statistics, it’s more important than ever for everyone to understand what a heart attack is, what physically happens in the heart, how to spot early signs, and how prevention really works. In this article, we’ll walk through the anatomy and physiology in a way that you (and your readers) can visualize—especially with 3D modes in mind—while keeping it simple and actionable.
What Is Cardiovascular Disease (CVD)?
Cardiovascular disease (CVD) is an umbrella term for conditions that affect the heart or blood vessels. Some of the major types include:
Coronary artery disease (CAD) (narrowing or blockages in coronary arteries)
Heart attacks (acute blockages causing heart muscle damage)
Stroke (blockage or breakage in brain blood vessels)
Arrhythmias (irregular heart rhythms)
Heart failure (when the heart cannot pump well)
Valvular heart disease (abnormal heart valves)
Because these conditions share many risk factors—like high blood pressure, high cholesterol, smoking, diabetes, obesity—their prevention often overlaps.
Global trends:
From 1990 to 2022, deaths from cardiovascular disease rose from ~12.4 million to ~19.8 million globally, largely due to aging and population growth.
Yet, in many countries, age-standardized death rates for CVD have declined due to better healthcare, awareness, and prevention.
In the U.S. alone, one person dies every 34 seconds from cardiovascular disease.
Between 1970 and 2022, deaths due specifically to acute heart attacks declined by nearly 90% (in age-adjusted terms), reflecting better treatments and early interventions.
So yes — heart disease is still the leading killer worldwide, but we’re also seeing progress thanks to medical advances and prevention efforts.
How Does the Heart Work?
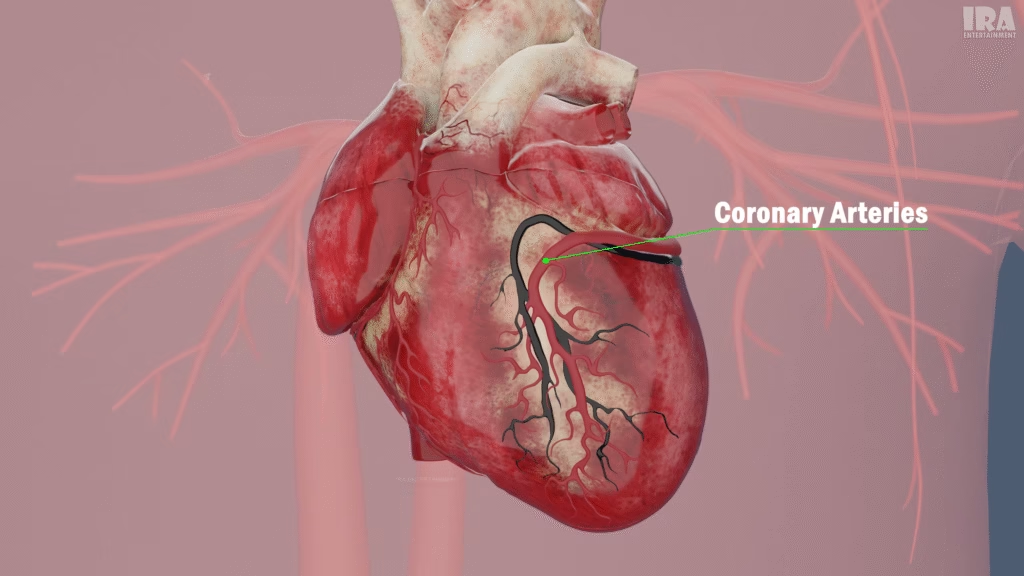
Just like every other cell in the body, heart muscles need a constant supply of oxygen and nutrients. This supply comes from special blood vessels called coronary arteries, which wrap around the heart like a complex network.
Here’s where the problem starts: over time, these arteries can become clogged due to the buildup of plaque, a substance made of fat, cholesterol, and other deposits. This narrowing of arteries is known as atherosclerosis.
The Pathology: From Plaque to Heart Attack
What is atherosclerosis?
Atherosclerosis is the underlying disease process that sets the stage for most heart attacks. In simple terms:
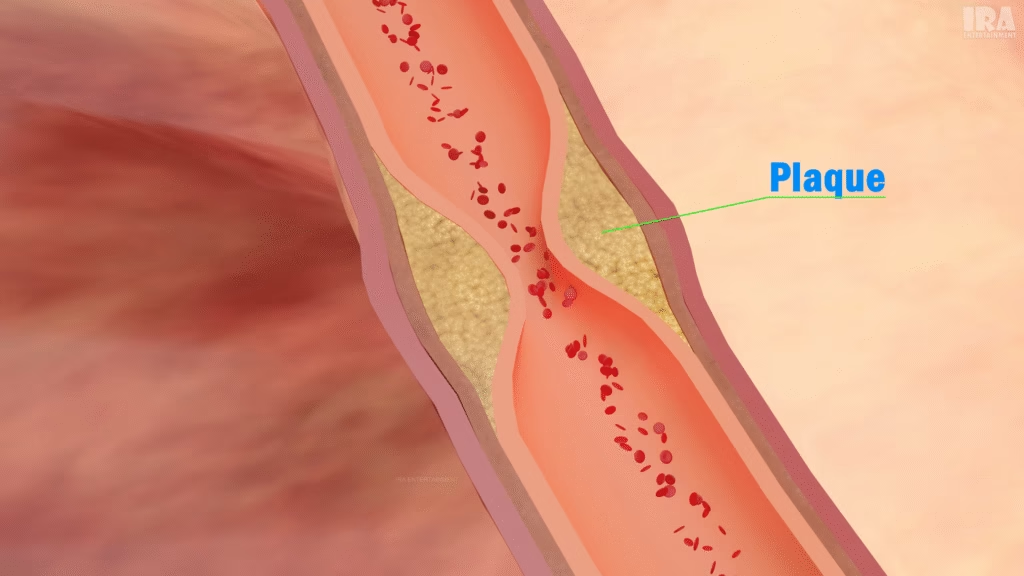
Over years or decades, lipids (fats), cholesterol, calcium, inflammatory cells, and connective tissue deposit inside artery walls.
This forms a plaque (fatty, hardened deposit) that narrows the artery’s lumen (the open channel).
The artery walls become stiffer and less elastic.
When the plaque surface cracks (rupture), it triggers blood clotting, leading to sudden and dangerous blockages.
Risk factors for plaque buildup
Three major culprits:
High blood pressure (hypertension): Repeated high pressure damages the inner lining (endothelium) of arteries, making them more vulnerable.
High cholesterol / lipid disorders: Excess “bad” LDL cholesterol tends to accumulate in artery walls.
Smoking: Tobacco and its chemicals injure the lining, accelerate inflammation, and promote clotting.
Additional contributors include:
Diabetes and insulin resistance
Obesity (especially abdominal fat)
Sedentary lifestyle
Unhealthy diet (high in saturated fats, trans fats, refined sugars)
Chronic stress
Genetic predisposition
Modern research also links air pollution to increased risk of atherosclerosis and acute cardiovascular events.
Plaque rupture and thrombosis
Plaques may remain stable for years, causing mild symptoms (like angina) or none at all. But the most dangerous moment is when a plaque ruptures:
The tear exposes internal contents to the bloodstream.
Platelets rush in and form a clot (thrombus) to patch the rupture.
That clot can block the artery fully or partially.
The downstream portion of the heart muscle loses blood flow — ischemia occurs.
If blood flow isn’t restored quickly, infarction (tissue death) results.
Heart Attack vs. Cardiac Arrest
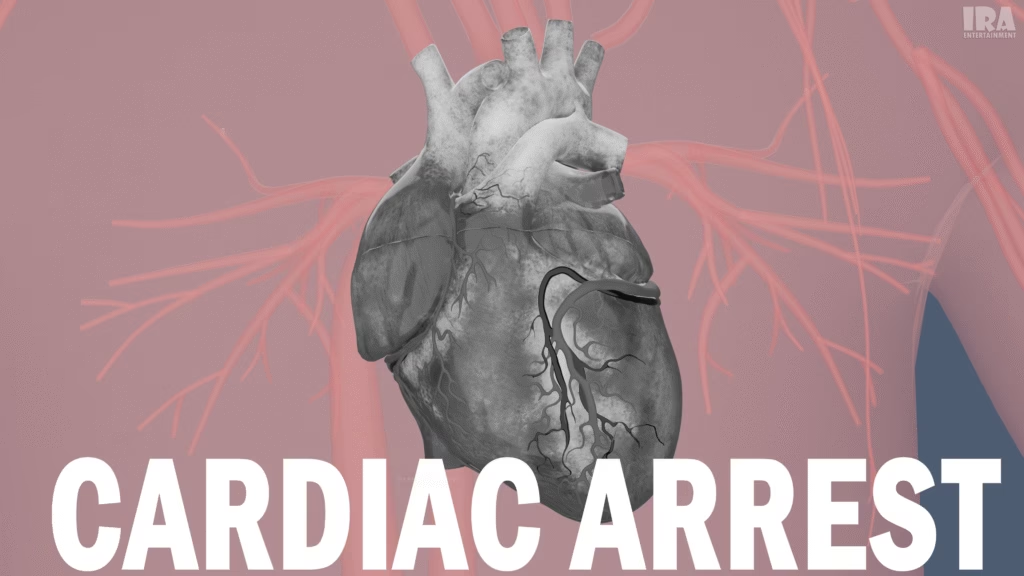
These terms are often confused, but they represent different events:
Heart Attack (Myocardial Infarction): A blockage in a coronary artery leads to death of cardiac muscle tissue. The heart still beats (though sometimes abnormally).
Cardiac Arrest: The electrical system fails, causing the heart to stop pumping (ventricular fibrillation or asystole). Without immediate help (CPR, defibrillation), this leads to death.
A heart attack can lead to cardiac arrest, but not all cardiac arrests begin as heart attacks.
Common Symptoms of a Heart Attack
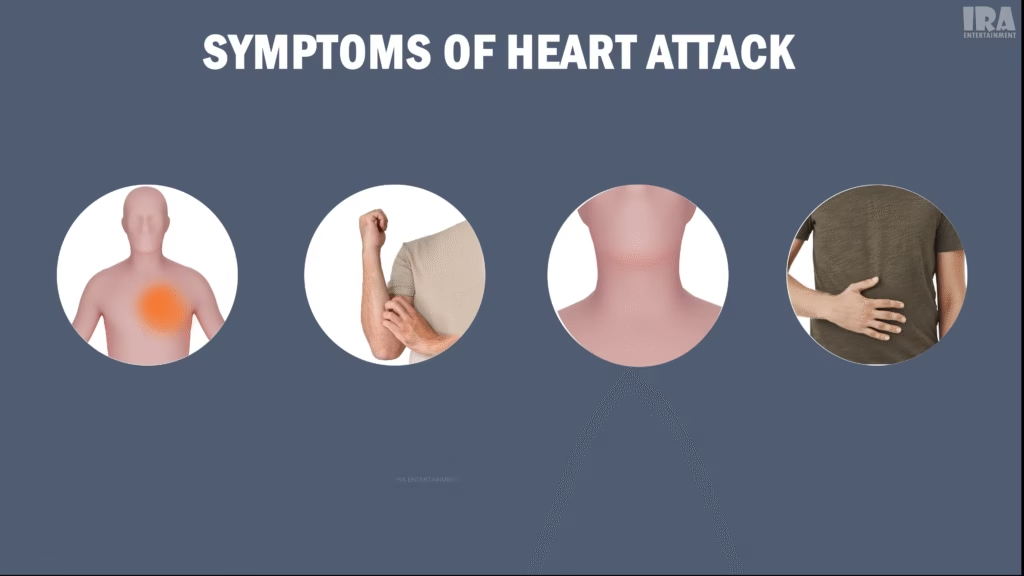
Recognizing symptoms early can save lives. Symptoms vary by person (men vs women, younger vs older) and may be subtle.
Common signs include:
Chest discomfort or pressure (often described as squeezing, fullness, or heaviness)
Pain or discomfort in one or both arms (or shoulders)
Pain in neck, jaw, back, or upper stomach
Shortness of breath (with or without chest discomfort)
Unexplained sweating, cold sweats
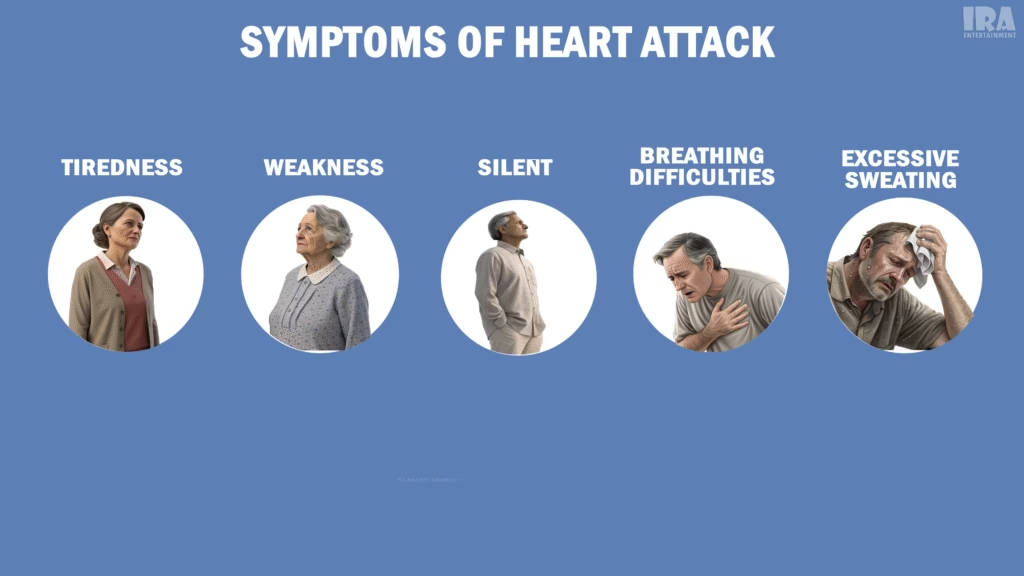
Weakness, lightheadedness, fatigue
Nausea or indigestion
In some cases, particularly among women, older adults, and people with diabetes, symptoms may be atypical or “silent” (no obvious chest pain).
It’s estimated that 1 in 5 heart attacks is “silent”, meaning the person does not realize they’ve had one until it’s seen on ECG, imaging, or tests.
As soon as you suspect a heart attack—yourself or someone else—call emergency services immediately. Time is muscle: the longer cardiac tissue is deprived of blood, the more damage.
Diagnosing a Heart Attack
Modern medicine provides several tools to diagnose a heart attack quickly and accurately:
Electrocardiogram (ECG / EKG): Detects electrical changes in heart muscle, such as ST elevation (STEMI) or non-ST elevation (NSTEMI).
Cardiac biomarkers (blood tests): Troponin and CK-MB levels rise in the blood when heart muscle is damaged.
Echocardiography (ultrasound): Assesses heart wall motion abnormalities, which might point to a region of damage.
Coronary angiography / cardiac catheterization: A contrast dye is injected to visualize blockages in coronary arteries (often in 3D imaging).
CT angiography: Noninvasive imaging of coronary arteries.

How Doctors Treat Heart Attacks
Once a diagnosis is confirmed, the goal is to restore blood flow and limit damage. Here are key interventions
1. Clot-busting drugs (Thrombolysis / Fibrinolysis)
Medications (e.g. tPA, streptokinase) dissolve the clot to reopen the artery. Best used early when angioplasty isn’t immediately available.
2. Percutaneous Coronary Intervention (PCI / Angioplasty)
A catheter is inserted into the artery (often via the wrist or groin). A balloon is inflated at the blockage to compress the clot and plaque. Then, a stent (a tiny mesh tube) may be placed to keep the artery open.
3. Coronary Artery Bypass Grafting (CABG)
In more complex blockages, surgeons may use veins or arteries from elsewhere in the body to bypass (go around) blocked coronary arteries.
4. Medications for stabilization
After the acute phase, ongoing treatments include:
Antiplatelet drugs (aspirin, P2Y12 inhibitors) to prevent further clots
Statins to lower LDL cholesterol
Beta blockers, ACE inhibitors / ARBs to reduce workload on the heart
ACE/ARB helps with remodeling and reducing further damage
Lifestyle modifications (see prevention section below)
A recent study indicated that combining statins with ezetimibe shortly after a heart attack can further reduce future risks
Recovery and Remodeling
After a heart attack, the heart begins a healing process:
The dead tissue is gradually replaced with scar tissue (non-contractile).
The heart may remodel (change shape) to compensate, which sometimes leads to heart failure if the remodeling is unhealthy.
Rehabilitation (cardiac rehab) helps patients regain strength and adapt to life after MI.
Preventing Heart Attacks
While heart attacks are serious, many can be prevented by adopting heart-healthy habits:
1. Healthy diet
Focus on whole grains, fruits, vegetables, lean proteins, and healthy fats (e.g., omega-3s).
Reduce saturated fats, trans fats, processed foods, added sugars, excess salt.
2. Regular exercise
Aim for 150 minutes of moderate-intensity physical activity weekly (e.g., brisk walking).
Add strength training 2–3 times per week.
3. Quit smoking & avoid secondhand smoke
4. Maintain healthy weight
Especially reduce visceral (belly) fat.
5. Monitor & control medical conditions
Keep blood pressure under control
Manage cholesterol (especially LDL)
Control diabetes / blood sugar
Address sleep disorders (like sleep apnea)
Control stress through relaxation, mindfulness, therapy
6. Regular screening & checkups
Interestingly, some researchers are now using machine learning models to predict heart attack risk in vulnerable populations, combining demographic, biochemical, ECG, and stress-test data.
Most heart attacks and strokes are considered largely preventable if risk factors are managed early.

Early Warning Signs & How to Act
Knowing early signs is critical. Some people experience prodromal symptoms hours to days before a full-blown heart attack.
Possible warning signs:
Mild chest discomfort or pressure that comes and goes
Shortness of breath
Unexplained fatigue or weakness
Indigestion or nausea
Cold sweats
Lightheadedness
In a recent study, over 99% of heart attack patients had at least one early warning sign or risk factor detectable well before the event.
What to do:
Don’t ignore mild chest discomfort — act early.
Call emergency services immediately if you suspect a heart attack.
Chew one adult aspirin (if you’re not allergic) while waiting, unless instructed otherwise.
Stay calm, sit or lie down, avoid exertion until help arrives.
Special Considerations: Women, Diabetes & Older Adults
Women often present with more subtle or atypical symptoms (nausea, jaw or neck pain, fatigue) rather than classic chest pain.
People with diabetes may have silent heart attacks more often because nerve damage dulls pain signals.
Older adults may discount symptoms as just “old age” or another condition.
In these groups, high vigilance is essential—regular checkups and awareness matter.
Complications After a Heart Attack
Heart attack survivors face a range of possible complications:
Arrhythmias (irregular heartbeats)
Heart failure if the heart’s pumping ability is weakened
Ventricular aneurysm (a bulge in the weakened muscle)
Pericarditis (inflammation of the heart’s outer lining)
Cardiogenic shock (when heart can’t pump enough blood to organs)
Recurrent heart attacks
Medical care and lifestyle changes can help mitigate these risks significantly.
Protecting the Heart That Keeps You Alive
Heart attacks are not sudden random events—they’re often the result of years of silent damage inside the arteries. By understanding what happens inside your heart, you gain the power to act before it’s too late. Regular checkups, a balanced diet, physical activity, and stress management can make a life-changing difference. Modern medicine and 3D visual technology now allow us to see heart health more clearly than ever before, turning awareness into prevention and prevention into action.
Your heart works tirelessly for you every second—take care of it today, and it will take care of you for a lifetime.
About the Author
This article was prepared by the IRA Studios editorial team, creators of high-quality 3D educational visualizations designed to simplify complex ideas through clear and engaging visuals.
Watch the Full 3D Animation
To explore all of these processes in 3D, check out our detailed 3D Animation video.
Watch it in Malayalam
Want to learn more through visual storytelling? Check out our detailed 3D explanation blog on What Is a Cesarean Delivery (C-Section)?
Useful Link : Myocardial infarction
Nice
Thank You!